Basal thumb arthritis is a very common condition mainly affecting middle aged women but also men who perform manual tasks. It presents with pain at the base of the thumb and difficultywith everyday tasks such as opening tight jar lids, pain on wringing out a cloth and difficulty holding objects such as a kettle.
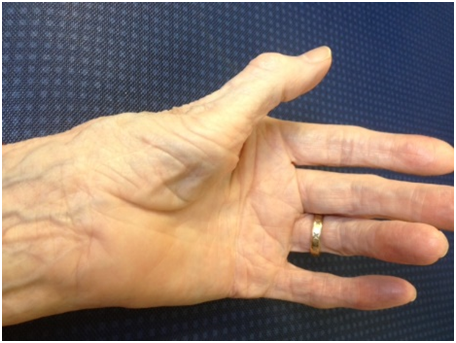
The condition is confirmed by expert examination – pain and crepitus on grinding or axially loading the thumb. As the disease progresses the hand can adopt a characteristic appearance as the basal thumb joint gradually subluxes and the thumb adducts with secondary compensatory hyperextension at the metacarpophalangeal joint resulting in a Z thumb deformity in advanced cases.
XRs will usually confirm the diagnosis. Occasionally, the XRs will show that the at the joint below (the scaphotrapeziotrapezoidal joint,STTJ ) is also arthritic.
Treatment is tailored to the severity of disease. In mild cases lifestyle modification, simple analgesia and possible splintage may suffice. In others, a steroid injection into the basal thumb joint can be helpful. In fact the majority of patients who get as far as presenting to a hand surgeon will probably have a steroid injection as most will have already tried the simpler treatments. The risks of steroid injections are post-steroid flare, depigmentation and skin atrophy. Yours surgeon will discuss these with you.
Surgery when all other treatments have failed
There are 2 surgical options for base of thumb arthritis – trapeziectomy (and LRTI – ligament reconstruction tendon interposition) or the newer joint replacement (MAIA) . The jury is out as to which is best but there are differences in the technical procedure , risks , rehabilitation on and benefits It is important that the surgeon discusses both options with the patient ,
Overview
The trapeziometacarpal joint, located at the base of the thumb, is commonly affected by osteoarthritis, causing pain, stiffness, and reduced function. Surgery is considered when non-surgical treatments (e.g., splints, injections, therapy) fail to relieve symptoms. Two common procedures are:
Trapeziometacarpal Joint Replacement
Description:
The damaged TMC joint surfaces are removed, and an artificial joint (prosthesis) is implanted. The prosthesis typically consists of a metal stem in the metacarpal and a socket component replacing the trapezium.
Anaesthesia: General or regional (nerve block which makes the arm numb).
-Duration: Approximately 1–1.5 hours.
-Hospital Stay: Usually same-day discharge
Rehabilitation
-Immobilization: A splint is worn for 2–4 weeks to protect the implant.
– Exercises: begin 2 weeks post-surgery, focusing on:
– Restoring thumb motion and strength.
– Preventing stiffness.
– Gradual return to daily activities.
– Recovery Timeline:
– Light activities (e.g., writing): 2-6 weeks.
– Full strength and heavy tasks: 6weeks to 3 months.
– Follow-Up: Check at 4-6 weeks monitor implant stability and ensure function improving.
Risks
– Implant-Related:
– Loosening or wear of the prosthesis over time (may require revision surgery).
– Dislocation of the implant.
– Fracture during implantation may require conversion to trapeziectomy
– General Surgical Risks:
– Infection (1–2% risk).
– Nerve or blood vessel injury (rare).
– Persistent pain or stiffness.
– Long-Term: Studies currently show that approximately 85-90% of implants are still functioning well after 12 years. There is a risk of needing further surgery at a later date.
Benefits
– Pain Relief: Significant reduction in thumb pain.
– Function: Improved thumb motion and grip strength compared to trapeziectomy in some studies.
– Stability: Maintains thumb length and alignment, potentially reducing deformity.
– Recovery: Potentially faster return to function than trapeziectomy due to preserved joint structure.
Trapeziectomy (with or without Ligament Reconstruction and Tendon Interposition – LRTI)
Procedure
– Description: The trapezium bone is removed, creating a space at the thumb base so that the worn joint surfaces do not rub against each other. In LRTI, a tendon (often from the wrist) is used to stabilize the joint and fill the space.
– Anaesthesia: General or regional.
– Duration: 1–1.5 hours.
– Hospital Stay: Typically discharge same day
Rehabilitation
-Immobilization: A splint is worn for 4–6 weeks.
– Therapy: Hand therapy starts 4–8 weeks post-surgery, focusing on:
– Restoring thumb mobility and strength.
– Preventing scar tissue formation.
– Recovery Timeline:
– Light activities: 8–12 weeks.
– Full strength: 6–12 months (longer than joint replacement).
– Follow-Up: Monitoring for thumb stability and function.
Risks
– Procedure-Specific:
– Thumb weakness due to loss of trapezium (may affect pinch strength).
– Instability or collapse of the thumb base (metacarpal subsidence).
– 5-10% of individuals unhappy with level of improvement
– General Surgical Risks:
– Infection (1–2% risk).
– Nerve or tendon injury.
– Complex regional pain syndrome (rare).
– Long-Term: No implant, so no risk of implant failure, but thumb shortening may occur.
Benefits
-Pain Relief: Effective long-term pain reduction in most patients.
– Durability: No prosthesis, so no need for revision due to implant wear.
– Proven Track Record: Widely performed with reliable outcomes over decades.
– Suitability: Ideal for older or less active patients, as it avoids implant-related complications.
Comparison
| Joint Replacement | Trapeziectomy | |
| Procedure | Replaces joint with prosthesis | Removes trapezium; may use tendon for stability |
| Pain Relief | Excellent in most cases | Excellent in most cases |
| Thumb Strength | Often better pinch/grip strength initially | May have reduced pinch strength long-term |
| Thumb Stability | Maintains thumb length and alignment | Risk of thumb shortening or instability |
| Recovery Time | Faster return to function (2-4 months) | Slower, full strength may take 6–12 months |
| Longevity | Implant may wear out unknown very long term outcome | No implant, so no wear; lifelong durability |
| Risks | Implant loosening, dislocation, revision surgery | Weakness, instability, thumb collapse |
| Ideal Candidate | Younger, active patients needing strength. Little or no arthritis in joint below. | Older or less active patients |
Additional Information
– Non-Surgical Alternatives: Before surgery, consider splints, physical therapy, or corticosteroid injections. These may delay or avoid the need for surgery.
– Post-Surgery Care: Follow your surgeon’s and therapist’s instructions to optimize recovery and minimize complications.
– Questions for Your Surgeon:
– Which procedure is would you recommend for my specific condition?
– What is the expected recovery timeline for my lifestyle?
– How many of these procedures have you performed?